A diabetic 55 years old lady with a history of breast cancer presented to me with visual loss in her left eye.
Fundus image
Her fundus exam shows chorioretinal elevation in the superior temporal quadrant with pigmentary changes and intraretinal blood. In contrast, the left eye examination shows multifocal retinal serous detachments at the macula and inferior retinal quadrants.
 |
| Fundus image of the Right Eye |
 |
| Fundus image of the Left Eye showing RD from exudative metastatic choroidal mass |
Optical coherence tomography
OCT of the right eye shows an elevation of the chorioretinal complex with subretinal fluids due to metastatic mass. In contrast, the left eye OCT scan shows an elevation of a choroidal retinal complex with massive subretinal fluids and some intraretinal cysts.
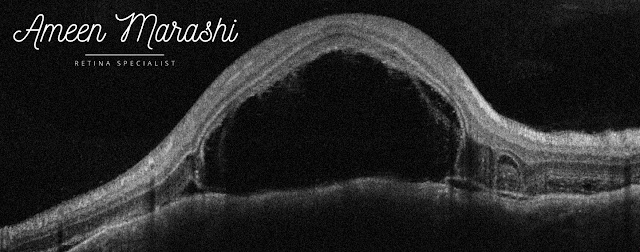 |
| OCT cross-section showing choroidal mass altering chorioretinal contour with subretinal fluids |
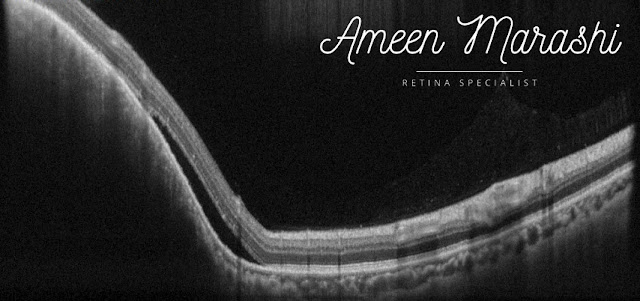 |
| OCT cross-section showing choroidal mass altering chorioretinal contour with subretinal fluids |
Diagnosis is choroidal metastasis in the right eye while the left eye is serous retinal detachment due to choroidal metastasis.
Differential Diagnosis
-Choroidal amelanotic melanoma -Posterior scleritis -Choroidal osteoma
-Harada
-Central Serous Retinopathy
Management
Systemic chemotherapy along with plaque radiculopathy
Discussion
This lady was diagnosed with breast cancer and managed with mastectomy and hasn't been followed up for years. Her diabetes has nothing to do with current pathology and detachments. This case shouldn't be confused with amelanotic melanoma as metastasis due to a history of primary breast cancer and presented as unifocal and pigmentary changes. At the same time, Posterior scleritis features pain and choroidal folds, which are absent in this case.
This case is easily differentiated from central serous retinopathy due to general thin choroidal profile (in except area of the choroidal mass area) and the intraretinal cystic formation, and finally, this cannot be mistaken with Harada due to the natural history of the patient and elevation of the choroidal retinal complex is the prominent feature rather than multifocal serous retinal detachments.
Management usually should be done with chemotherapy under an oncologist's supervision, and pars plana vitrectomy is NOT indicated.
You have provided valuable data for us. It is great and informative for everyone. Keep posting always. I am very thankful to you. eye specialist in Houston
ReplyDelete