A patient presented with dyschromatopsia and photophobia with reduced vision to hand motion (HM)
Fundus image
Fundus exam shows golden sheen of the macula atrophic changes.
 |
| Fundus image showing cone-rod dystrophy golden sheen refelex with atrophic changes |
Optical coherence tomography
OCT scan shows diffuse ellipsoid zone disruption and RPE atrophy, inducing increased reflectivity of the choroid. Although the fovea appears with normal contours, the boundaries between retinal layers are not clear.
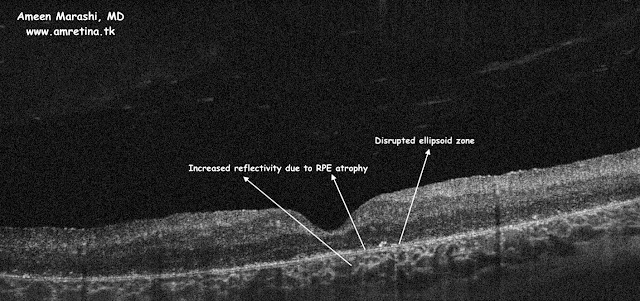 |
| OCT cross-section showing RPE atrophy with ellipsoid zone disruption in cone-rod dystrophy |
Discussion
This patient has bad BCVA of HM due to cone-rod dystrophy, which can be autosomal recessive, dominant, or X-linked disease. They usually suffer from dyschromatopsia and photophobia, in late-stage cone-rod dystrophy can cause legal blindness.
The quality and reliability of NewsPublicHealth’s content are outstanding. Their updates are always relevant and backed by credible sources. I appreciate how NewsPublicHealth contributes to increasing public awareness and helps people make informed health decisions.
ReplyDeleteNewsNoisy is simply outstanding for news lovers. Their commitment to delivering fast and factual information is unmatched. The website design is sleek, making reading effortless. I highly recommend NewsNoisy to anyone who values trustworthy news.
ReplyDelete