Polypoidal choroidal vasculopathy is a spectra of pachychoroid
Fundus image
In clinical practice, PED can occur in cases of PCV which features a radish-orange rounded punched from the choroid into the subretinal area with a possible association of subretinal hemorrhage or serous fluid accumulation.
 |
| Fundus image showing PCV with subretinal fluid |
Optical coherence tomography
OCT dome-shaped or M-shaped configuration on OCT and visible choroidal polyps well adhered to RPE which may have clear fluid or hemorrhage beneath it, with prominent Bruch’s membrane (in case absence of blood) forming double layered sign along with intraretinal and subretinal fluid.
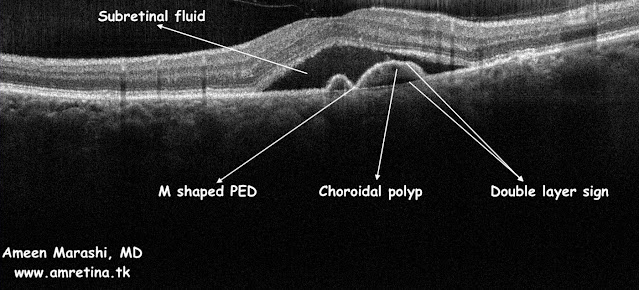 |
| OCT Cross-section showing PCV in M shaped PED and double-layer sign with subretinal fluid |
Fluorescein angiography
FFA shows hyperfluorescence may look similar to fibrovascular PED with hyperfluorescence notch resembling polyps surrounding subretinal dye pooling and maybe a combined with RPE atrophy inducing window defect.
 |
| Early phase FFA showing stippled hyperfluorescence with hyperfluorescence notch resembling PCV |
 |
| Mid phase FFA showing increased hyperfluorescence of the notch |
 |
| Late phase showing both subretinal and sub RPE pooling with leak from the PCV |
Management in a nutshell
PCV responds to AntiVEGF, such as Ranibizumab and Bevacizumab. If it failed to respond, then a VEGF trap such as aflibercept can be used and may require a combination of half-dose PDT in refractory cases.
Comments
Post a Comment