A 55 years old male known to be hypersensitive complains of reduced vision to HM in his left eye eight days ago. There is no other ocular nor systemic history except for an old corneal scar. Still, another colleague gave the patient dexamethasone intramuscularly, and he reported that he did MRI, and it is clear.
Fundus image
The fundus exam shows optic disc edema with star-shaped exudates at the macula.

Fundus image showing neuroretinitis with optic disc edema and hard exudates in a star shape 
Fundus image showing neuroretinitis with optic disc edema
Fundus fluorescein angiography
The FFA is done one week ago, showing leakage from the edematous optic disc.

Early FFA showing hyperfluorescence of the optic disc 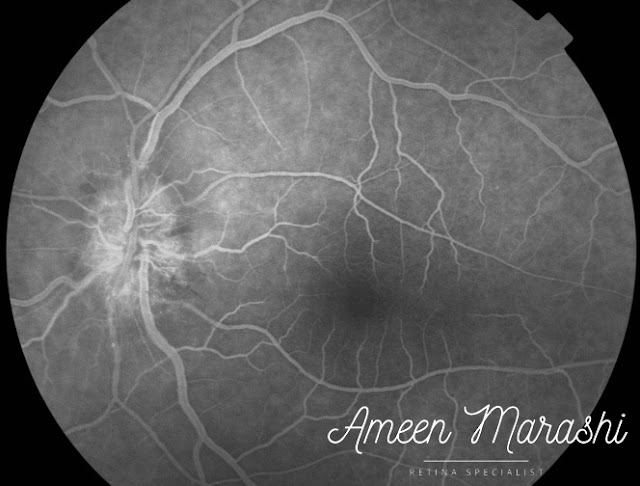
Mid FFA phase showing early leakage of the optic disc
 |
| Late FFA phase showing leakage of the optic disc |
Optical coherence tomography
Today he presented to me, and I have done OCT, and it shows central subretinal fluid with intraretinal hyperreflectivity that indicates hard exudates.
 |
| OCT cross-section showing subretinal fluids |
My Diagnosis is neuroretinitis.
Let us review neuroretinitis in a nutshell.
Pathology
Direct invasion of autoimmune activation leads to vascular inflammation of the optic nerve and edema in the RNFL. The exudative nature of the lipid-rich component can reach the outer plexiform layer.
At the same time, the aqueous phase can penetrate the external limiting membrane and form subretinal fluid.
Classification: infectious or idiopathic
Etiology
- Infectious, the most causative agent is Bartonella species, which can be accompanied by systemic features such as swollen lymph nodes, fatigue, headaches, and of course, fever. Other causative agents are syphilis, Lyme disease, Rocky Mountain Spotted Fever, toxoplasmosis, toxocariasis, histoplasmosis, and leptospirosis.
- Idiopathic has no clear causative agent nor mechanism, but flu-like symptoms could accompany it.
Symptoms
Patients may exhibit a painless decrease in central vision, decreased color vision, or, occasionally, may be asymptomatic.
Treatment
If the cause is a cat scratch, then antibiotics can be started, such as azithromycin or sulfamethoxazole-trimethoprim for children.
For the idiopathic variety, high-dose oral corticosteroids have been administered.
Please tell me about your recommendation.
Comments
Post a Comment