An 81 years old man pseudophakic presented to me with features of ARMD; his BCVA is 20/200 in his Right eye, while in his left eye, the BCVA is 20/35; fundus examination showed drusen and signs of ARMD.
Fundus image
Fundus examination shows drusen, RPE elevation, and subretinal fluid.
 |
| Fundus image shows fibrovascular PED with reticular pseudodrusen |
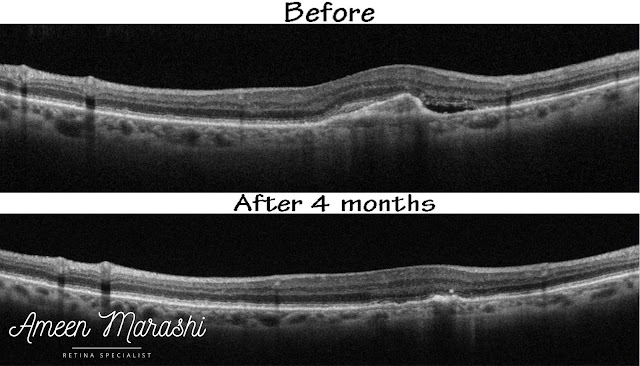
Optical coherence tomography
OCT cross-sections show RPE detachment area induced by a fibrovascular membrane with pronounced Bruch’s membrane forming double layered sign and subretinal fluid along of disturbed ellipsoid zone.
Diagnosis: This is a case of wet ARMD with occult choroidal neovascularization.
Management: This patient managed with monthly intravitreal Aflibercept for three consecutive injections and one-month post-treatment OCT cross-section shows resolving both subretinal fluid and fibrovascular PED and improved vision to 20/50, and the patient was followed up using PRN protocol.
Discussion
Wet ARMD can present as occult Choroidal neovascularization, which features a vascular proliferation sub RPE, and this proliferation may detach the RPE and induce PED and subretinal fluid, causing disturbance of outer retinal layers (ellipsoid zone),
Subretinal fluid and occult choroidal CNVm have a better visual prognosis than classical choroidal neovascularization, and intraretinal cyst may have a worse prognosis due to subretinal scar formation and intraretinal tissue disorganization.
This case treated with intravitreal Aflibercept for three consecutive monthly injections and one-month post-treatment OCT shows improvement in PED regression showing regression of the fibrovascular membrane and reducing in size and resolved subretinal fluid with BCVA improved to 20/50 and not better due to the disturbed ellipsoid zone.
Please tell me how you would manage this case in your clinical practice??!!!
Comments
Post a Comment