A 38 years old lady known for secondary hypertension due to adrenal gland dysfunction (as described by the patient) complains of sudden reduction of vision for the last two weeks in her left eye.
BCVA 20/80 in the left eye while 20/20 in the right eye has unremarkable anterior and posterior segment examinations.
Fundus image
The left eye anterior segment examination is unremarkable. The fundus exam showed radish elevated lesion (sub-ILM hemorrhage) in the fovea with mild vascular tortuosity, arteriolar constriction, and arteriovenous crossing.
 |
| Fundus image shows subILM hemorrhage |
Optical coherence tomography
OCT cross-section scan shows a hyperreflective mass in the sub ILM space, with shadow artifact hindering external retinal layers. Other retinal tissue findings on OCT are normal.
 |
| OCT cross-section shows subILM hemorrhage in the form of hyperreflective mass at the inner retinal layers |
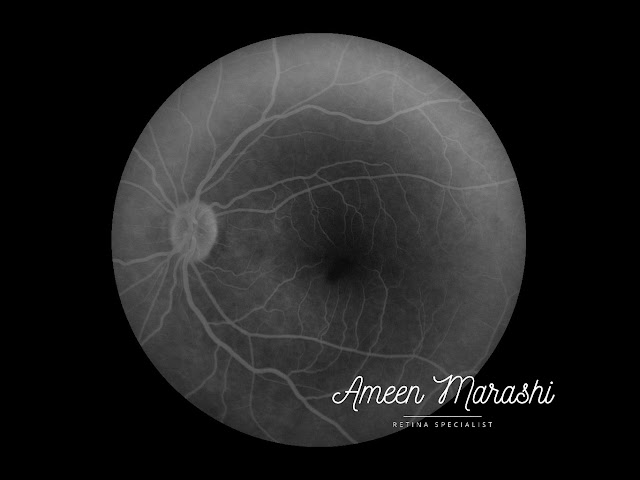
Fluorescein fundus angiography
Fluorescein angiogram shows hypofluorescence in the sub-ILM hemorrhage area masking the underling macular tissues in all phases, and there are no signs of perifoveal vascular abnormalities.
Early phase of FFA shows blocked fluorescence due to subILM hemorrhage
 |
| Mid phase of FFA shows blocked fluorescence due to subILM hemorrhage |
 |
| Late phase of FFA shows blocked fluorescence due to subILM hemorrhage |
Routine blood analysis is unremarkable and has been sent for internal specialist consultation for control of hypertension.
Discussion
The sub ILM hemorrhage is due to rupture of perifoveal capillaries caused by rapid changes in intraocular venous pressure; thus can be caused in Valsalva maneuver, sneezing, or coughing. However, other reasons for sub-ILM hemorrhage could be blood dyscrasia.
Usually, it takes weeks to several months to be completely resolved.
In cases where sub ILM hemorrhage is big enough to obscure the entire fovea, Yag laser, Intravitreal injection of tPA proceeded by pneumopexy, or simply intravitreal gas injection are indicated.
In this case, blood screening is unremarkable. The patient already suffers from blood hypertension, which is followed up by the internist. The hemorrhage's radish color is due to some blood cells becoming dehemoglobinized, and as it is not obscuring the entire macula, a decision was made to wait for spontaneous resolution.
In case it persists, then Intravitreal gas injection to displace the hemorrhage as YAG is not safe to be done due to its flat and close proximity to FAZ profile to avoid potential complications such as a macular hole.

The information which you have provided is very good and essential for everyone. Keep sharing this kind of information. Thank you. houston retina specialists
ReplyDelete