Fifty-six years old male complains of painless onset reduction of vision in his right eye to CF. His other eye exam is normal. He has a systemic history of ongoing treatment for bronchial cancer.
Fundus image
His fundus photograph shows an area of elevated pale fovea with pigmentation surrounded by subretinal blood, hard exudates, and subretinal fluid. Another eye exam is normal, and the BCVA is 20/20.
 |
| Classical CNVm fundus image |
Optical coherence tomography
His OCT shows increased retinal thickness with intraretinal cyst formation, which disturbed both the ellipsoid zone and the external limiting membrane and subretinal fluid and blood. In contrast, this subretinal amorphous material represents a choroidal neovascular membrane complex.
 |
| OCT scan of classical CNVm showing SHRM and SRF |
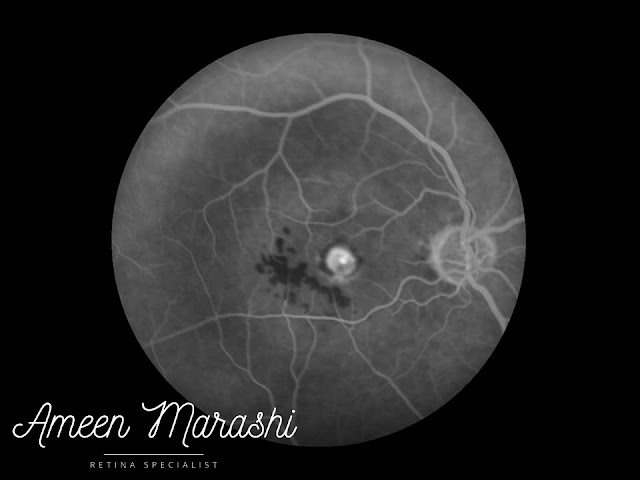
Fundus fluorescein angiography
His FFA shows in the early phase (Arteriovenous phase) shows hypofluorescence due to blockage from subretinal blood (please note how the patient couldn't fixate centrally due to acute compromised central vision). However, in the mid-phase, a hyperfluorescence of classic CNVm with well-defined edges can be noted, where the late phase shows a leak from the classic CNVm and pooling of dye in the subretinal fluid.
 | ||
Early phase of FFA showing hyperfluorescence from Classical CNVm
|
 |
| Late phase showing leakage from classical CNVm |
Diagnosis
Diagnosis is classic choroidal neovascularization, which proliferates in the subretinal space in contrast to occult choroidal neovascularization, which proliferates in the subRPE space.
Management
Treatment is by monthly injecting VEGF blockage agents, follow up should be done using OCT if CNVm regression occurred then pro re nata or treat and extend protocol should be applied.
Classic CNVm usually has a worse prognosis than occult CNVm because of subretinal scar formation and photoreceptor destruction.
Comments
Post a Comment