A 63 years old lady systematically free presented with symptoms of floaters of her right eye minimally distorted vision BCVA in her left eye 20/25, and her vision in the left eye is 20/20.
Her left eye's clinical examination: anterior and posterior segment unremarkable while her right eye the anterior segment exam is unremarkable, her fundus exam shows some vitreous opacities and abnormal macular and irregular foveal reflex.
Fundus image
Fundus colored photograph shows wrinkling of the internal limiting membrane (ILM) and epiretinal formation with vascular tortuosity forming a cellophane maculopathy. However, the fovea has an abnormal shape with suspicion of a macular hole; some of the fundus' anatomical features are masked due to vitreous opacities.
 |
| Fundus image showing epiretinal membrane forming macular pseudohole |
Optical coherence tomography
OCT scan shows vitreomacular abnormalities in the form of an epiretinal membrane with minimal focal disturbance of inner retinal tissues with abnormal foveal contours with no disturbance of external limiting membrane nor ellipsoid zone, with a slight increase of retinal thickness.
 |
| OCT cross-section showing macular pseudohole |
The enface image in the Vitreous/ILM level shows an epiretinal membrane with a smooth central circle with a central hyporeflective circle presenting the epiretinal membrane's hole.
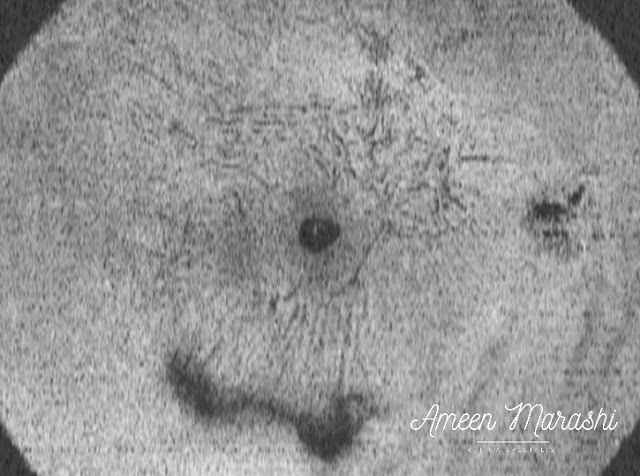 |
| Enface OCT showing Vitreous/ILM slab featuring macular pseudohole |
Diagnosis: Macular Pseudohole
Management: Follow up as BCVA is 20/25
Discussion
Epiretinal membrane forms when a schisis of the posterior cortical vitreous occurs in the PVD process, explaining the vitreous opacities. The remnant of the cortical vitreous will induce glial proliferation, which can cause tangential traction. In this case, there is no full-thickness retinal defect. Instead, a gap in the epiretinal membrane appears as a macular hole with thickened retinal tissue around the abnormally-shaped fovea. In contrast, the lamellar hole may or may not feature an epiretinal membrane with cleavage of inner retinal layers and foveal cavity with undermined edges with or without cystic changes with an irregular lamellar split of the outer retinal layers at the fovea or without intact ellipsoid zone. However, full-thickness macular hole, presented with a full-thickness foveal defect in the stages 2,3,4 and usually as the vitreomacular traction is the main pathological factor.
Clinically the pseudohole has better visual outcomes than the lamellar hole, but pseudohole can be transformed into a lamellar hole, and PPV indicated in cases with poor visual acuity
A full-thickness hole can be presented with poorer visual acuity and may require pars plana vitrectomy with ILM peeling.
You have done great work by publishing this article here. It is useful and convenient info for us. Keep upgrading our knowledge by share these types of articles.Pterygium Houston
ReplyDelete